In the same way that sheet music shows musicians what to play, DNA shows the body how to function. But what if a violinist’s pages got jumbled out of order, or the melodies marked mute? The instructions would still be there, but they wouldn’t make sense to the player.
By studying mouse models, scientists at the University of Wisconsin School of Medicine and Public Health have discovered how inflammation makes genetic instructions in muscle stem cells, or MuSCs, unreadable. DNA should tell the body how to regulate iron, so without those regulations, cells rust to death in a process called ferroptosis.
Iron is needed to make hemoglobin, a protein in red blood cells that carries oxygen throughout the body. It is also vital to a functioning immune system and repairing muscle tissue. The study, published in Nature Aging, has implications for understanding and potentially treating sarcopenia, which is the age-related loss of muscle mass and strength in humans.
“As we get older, the little repair workers in our muscles — called stem cells — start to disappear,” said Roméo Blanc, assistant professor of cell and regenerative biology at the UW, who led the study. “Iron is very helpful for your body, but old stem cells hoard so much of it that it becomes toxic. We found a way to help them stay safe and do their job again.”
In humans, muscle deterioration begins as early as age 30 and continues into old age, contributing to loss of function, disability and mortality.
Weakness and frailty often lead to falls. Every 20 minutes, an older adult dies from a fall in the United States.
“Right now, there’s no real way to prevent the decline of muscle mass with aging,” said Blanc.
His research team aims to change that.
Researchers began by analyzing blood from young and aged mice to determine cellular and molecular changes over time. They screened the mice for over 100 proteins related to inflammatory processes and analyzed muscle from the aged mice.
Aged muscle exhibited signs of inflammation. Computational predictions using blood and muscle data showed that a protein called the CCR2 receptor, which interprets inflammatory signals, was more active than usual. Scientists then induced inflammation in young mice with CCR2 signals to see the impact on MuSCs.
This showed them how the violinist’s pages got mixed up.
The dysregulation that occurs during inflammation and aging, dubbed “inflammaging,” affected Kmt5a — a key gene that helps configure and prioritize stretches of DNA as readable instructions for the body. A lack of Kmt5a activity during inflammation and aging showed researchers that this gene normally helps organize the body’s genetic instructions into something readable.
Kmt5a places small chemical tags, called methyl groups, onto specific parts of histone proteins that strands of DNA wrap around. Physically morphing the three-dimensional structure of DNA in the cell leads to changes in the DNA’s accessibility to the body
In this way, genes that protected against iron-related cell death were silenced, as were genes that keep muscle stem cells in a resting state, ready to help repair damaged or aging muscles. As a result, the cells stayed active when they should have been resting to stand ready for muscle regeneration when needed.
This constant activity, combined with the loss of iron regulation, causes muscle stem cells to wear themselves out and die from iron toxicity.
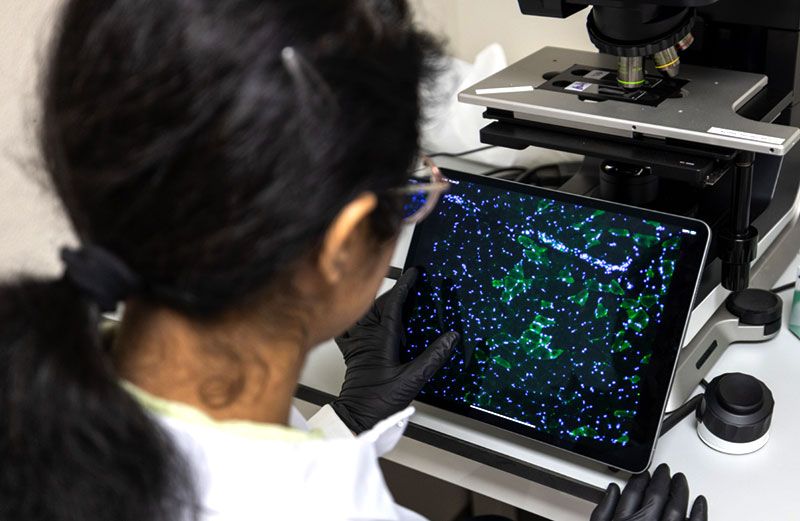
Scientists engineered mice to lack the Kmt5a gene in MuSCs, and in those mice, 28% of MuSCs showed signs of cell death and elevated DNA damage response. There are many ways a cell can die, and Blanc assumed the type of cell death would be common, but after single-cell RNA sequencing, he discovered cells dying through ferroptosis.
When iron processing is deregulated, MuSCs accumulate the iron, causing them to rust and weaken. The lipids, or fat, in the cell rot away. This same process occurs in naturally aging muscle stem cells.
Under normal conditions in mice, less than 2% of MuSCs have detectable iron accumulation within the cell, referred to as iron foci. In Kmt5a knockout mice, this figure jumped to 80%. Additionally, the level of iron in cells of mice lacking Kmt5a was 70 times higher compared to control muscle stem cells.
To test whether interrupting inflammation would affect iron-mediated cell death, scientists treated aged mice with an anti-inflammatory drug called Bindarit, hoping to prevent the epigenetic changes that lead to ferroptosis. Bindarit restored Kmt5a levels in aged mice to levels of adult mice, decreasing iron accumulation. Scientists did not observe any off-target effects on young mice, making them hopeful that the drug specifically addressed and corrected inflammaging.
While further study is needed to assess the link between inflammation, ferroptosis, and muscle stem cell regulation in human aging, the work of Blanc’s team has implications for understanding optimal management of iron levels in humans.
“We have a paradox where when you age, you have an iron deficit, which leads to anemia and higher inflammation,” Blanc said. “But you also have chronic accumulation of iron inside other tissues, including muscle and muscle stem cells.”
Approximately 14% to 18% of Americans take a supplement containing iron and roughly 10% of the population suffers from anemia, which is often treated by increasing iron intake.
Ferroptosis and iron accumulation within the brain are also connected to neurodegenerative diseases like Alzheimer’s, Parkinson’s and Huntington’s disease.
The Blanc lab is conducting three related studies: understanding the link between iron metabolism and aging, studying the relationships between iron and epigenetics at the molecular level, and examining how exercise affects iron metabolism and epigenetics.
“The more we know and understand about the reasons behind stem cell loss, the more likely we are to develop meaningful ways to prevent that loss,” Blanc said.
– Author Mary Bosch is a 2025–26 science communications intern at the School of Medicine and Public Health
The research was supported in part by startup funding provided by the University of Wisconsin-Madison, including the Department of Cell and Regenerative Biology and the Office of the Vice Chancellor for Research, the UW Carbone Cancer Center, and the UW–Madison Stem Cell and Regenerative Medicine Center. Funding was also provided by the Wedd Endowment Fund and the National Institute on Aging (K99/R00AG071736).

