People who participate will receive individualized test results and up to $675 for completing the three-year study. To participate, visit MyVapeCheck.com.
Although studies have examined the physical effects of vaping, virtually all have examined very short-term or cross-sectional effects. These studies are valuable but do not provide the same degree of evidence as a study that follows people who vape for multiple years.
The study, known as Vape Check, is a collaboration between the UW Health Preventive Cardiology Program and the UW Center for Tobacco Research and Intervention (UW-CTRI).
“This study will produce the most informative evidence to date on how long-term vaping affects cardiovascular and pulmonary health as well as disease risk,” said Dr. James Stein, professor of medicine and director of both the UW Health Preventive Cardiology Program and the UW Atherosclerosis Imaging Research Program. Stein will co-lead the project with the associate director of UW-CTRI, Tim Baker, who holds a doctorate in clinical psychology.
The study team will recruit 400 participants aged 21 and older who have vaped regularly for a year or more and do not currently smoke, as well as 200 age- and gender-matched control participants who do not vape or smoke.
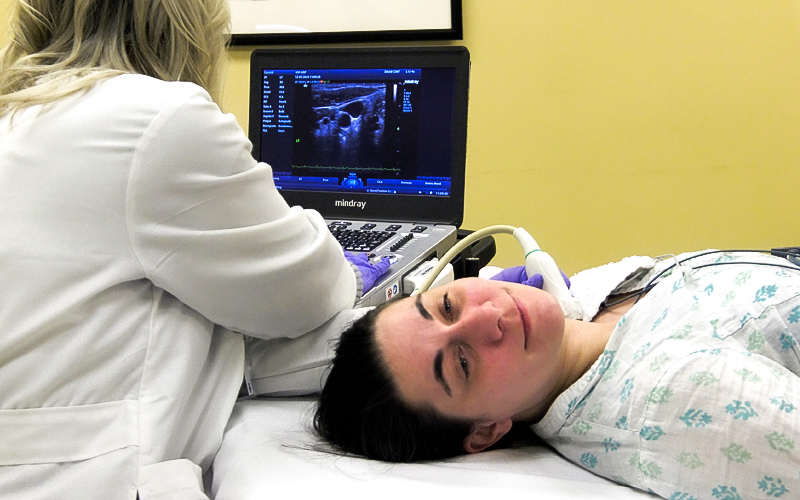
Participants will undergo comprehensive biomarker assessments at UW–Madison periodically over a span of three years.
Researchers will test vital signs, obtain non-fasting blood samples for inflammation and cardiometabolic health, and use ultrasound machines to check participants’ arteries for injury or other changes.