Science & Technology
January 13, 2026
Q&A: Christopher Sundberg on the role of muscles in the aging process
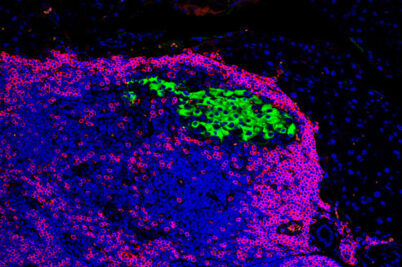
What determines healthspan, the term used to describe the number of years people live in good health and free from chronic disease? Muscle physiology plays a key role.