Education
February 11, 2026
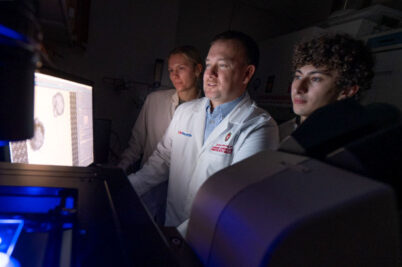
Preparing medical residents to practice lifestyle medicine
Americans are getting sicker earlier in life. More than half of young adults aged 18-34 years report at least one chronic condition, such as obesity or diabetes, and adults in midlife are increasingly likely to have two or more.