Science & Technology
January 29, 2026
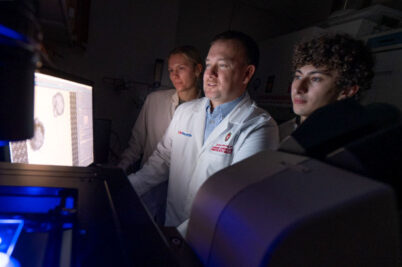
UW–Madison and Immuto Scientific to collaborate on novel cancer target discovery
University of Wisconsin–Madison and Immuto Scientific have officially entered into a collaborative agreement to identify disease-specific, novel therapeutic targets in colorectal cancer.