What is the potential impact of the vaccine, on patients’ lives and within the field of cancer research?
If successful, this will be a game changer for glioblastoma patients. Current median survival for the disease is between nine and twelve months and it has a recurrence rate of almost 100%. We can’t stop people from getting glioblastoma, but if the vaccine works in patients as it does in mouse models, we will essentially stop the disease from coming back.
We hope this vaccine may one day be adapted to treat other cancers in aging adults, since the basic mechanism of the vaccine is to boost one’s own immune system to target the cancer cells.
Is this vaccine close to a clinical trial?
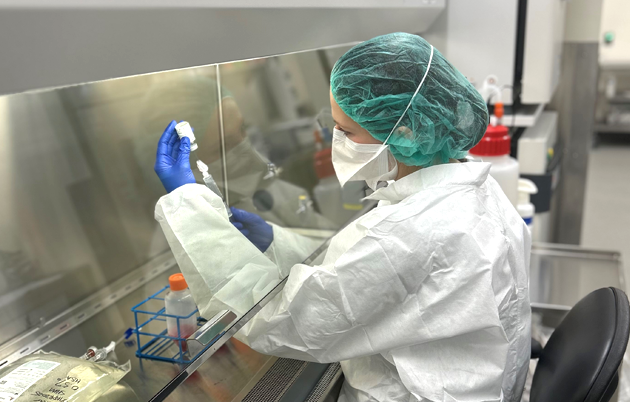
Our initial pre-clinical work showed that the vaccine is highly effective in multiple mouse models of glioblastoma. Since then, we have done in vitro testing of the human version of the vaccine and have found that patient-specific vaccines activate patients’ T-cells (protective white blood cells) for cytotoxic activity, or the ability to attack cancer. Now we are working on achieving good manufacturing practice (GMP) standards, ensuring quality and safety for human use. Once we create a GMP-grade vaccine, we will be ready to file for an investigational new drug application with the Food and Drug Administration to start a Phase I clinical trial. Our goal in that trial will be to evaluate the vaccine’s safety and determine dosage.
What are some of the unique challenges you face?
I get to know my patients and their families really well during their journeys, and eventually the treatments fail them. Many times, I take that as a personal failure, and it can be very demoralizing. However, I am very fortunate that many family members stay in touch with me even after the patient passes away, which makes me think that maybe I was able to make some difference in their lives. Another challenge of developing translational therapies is the complex coordination needed to bridge multiple disciplines. Over time I have learned to identify key collaborators and intentionally develop more in-depth work with them. Our vaccine work is a successful example of this focused, small-team strategy.
What motivates you to keep going in the face of setbacks?
If a goal doesn’t scare me and keep me up at night, then it’s not really a worthy goal. Science can be brutally heartbreaking at times. We do what we do because there are patients whose lives are cut short by this devastating disease. Our goal should always be to find a cure, and if we fail in that, we will at least end up increasing the survival rate.
How does your clinical practice inform your research, and vice versa?
To me, the role of surgeon-scientist is the best of all worlds — science meets humanity. As a surgeon, I remove brain tumors. As a scientist, I formulate and test hypotheses on what can be done to prevent this cancer from coming back. Each process feeds the other. Even though brain tumor patients face one of the worst cancer prognoses, they are often some of the most resilient and uplifting people I know. I find their courage and grace very motivational in my lab research.
Why is UW a great place to pursue your work?
UW is a complete ecosystem where one can take a basic science finding all the way to a clinical trial. When I was being recruited, I met with Dr. Jacques Galipeau, founding director of the Program for Advanced Cell Therapy. That meeting eventually led to a collaboration between our labs, and this vaccine is a direct result. I then had a serendipitous encounter with Jonathan Young, the chief scientific officer of WARF, and mentioned to him our very promising pre-clinical findings for the glioblastoma vaccine. WARF recognized the potential of our vaccine and the large unmet need for therapeutic development in the field of glioblastoma. This kind of multi-sector collaboration is a great example of what is possible at UW–Madison.