Phase 2 – MD Curriculum
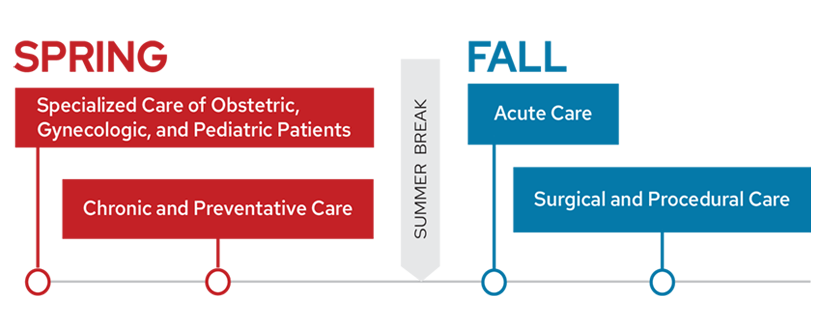
Phase 2 of the ForWard Curriculum consists of four, 12-week thematic blocks that emphasize clinical experiences and applications, fully integrating clinical care, basic science and thread topics.
Phase 2 Timeline
Phase 2 Blocks
Specialized Care of Obstetric, Gynecologic and Pediatric Patients
Specialized Care of Obstetric, Gynecologic and Pediatric Patients is a 12-week block in Phase 2 that is centered on the care of those populations, and emphasizes taking care of vulnerable populations, as well as working with caregivers.
It builds upon the fundamental science concepts introduced in Human Family Tree during Phase 1, such as embryology and teratology, genetic testing and neurodevelopment.
Clinical experiences occur in a range of settings such as pediatric primary care, labor and delivery, and obstetrics/gynecology. Structured educational sessions include a series of integrated case-based learning sessions that guide students to apply foundational concepts considering the unique needs and physiology of these patients. They employ varied modalities including podcasts, real-time case discussions, webcasts, independent readings and online nationally-supported modules.
Course Objectives
- Demonstrate an inclusive and humanistic approach to patient care
- Demonstrate the relevant foundational knowledge for the diagnosis and/or differential diagnosis
- Appropriately interpret objective data such as vital signs and commonly used diagnostic studies (including CBC, urinalysis, CSF analysis, serum chemistries), accounting for the age of the patient, presence or absence of disease, and testing modality employed
- Describe the appropriate use of the following common medications (accounting for age/weight and other patient factors), including when it is NOT appropriate to treat with these medications: analgesics, antipyretics, antibiotics, bronchodilators, corticosteroids, IV fluids
- Adapt your approach (medical interview and complete or focused physical examination) as is appropriate to your interaction with the patient and/or their caregivers, the patient’s age/level of development, as well as the presenting concern and clinical setting
- Generate an appropriate differential diagnosis and plan for the presenting problem and patient’s age
- Consider the invasiveness, benefits, limitations, costs, and evidence-based best practices when generating plans for patients in different clinical scenarios
- Develop familiarity with common procedures performed in obstetrics and gynecology inpatient and outpatient settings
- Responsibly manage information within the electronic health record (EHR) to effectively obtain and document patient care and utilize clinical decision support
- Actively participate as an interprofessional team member to promote patient care by fostering a positive learning environment and providing focused, actionable feedback
- Identify members of the health care team and describe how they contribute to the care of patients (nurse, pharmacist, respiratory therapist, PT, OT, speech therapy, child life, etc.)
- Develop an understanding for the ethical and medicolegal implications of working with patients of various ages and their proxies, including issues of capacity, competency, decision-making, guardianship, and confidentiality
- Develop an understanding for the physician’s role in mandated reporting and safety (including how it varies for patients of different ages) in cases of neglect and abuse (physical, sexual, verbal/psychological)
- Discuss ways to advocate for patients on an individual, community, regional, state or national level and consider barriers and health inequity pertinent to diverse populations
- Present the history, exam/objective data, assessment and plan for patients of all ages as is appropriate to the clinical scenario (patient problems and setting-clinic vs. inpatient, admission vs. follow-up, team vs. family-centered rounds)
- Document the history, physical examination, assessment and plan in a format appropriate to the clinical situation (clinic vs. inpatient; admission vs. progress; procedure notes), demonstrating best practices within the electronic health record
- Demonstrate effective communication strategies with a variety of audiences, including patients and families, to convey medical information and evidence-based healthcare recommendations while avoiding medical jargon
- Demonstrate integrity, organization, and dependability in all learning environments
- Identify community partners collaborators when advocating for pediatric and OB/GYN patients
- Counsel patients and/or their caregivers on plans that are appropriate to the patient’s age/development and their reason for presentation (plans may include appropriate anticipatory guidance, health maintenance, screening and prevention, treatment, supportive care)
- Promote effective communication to minimize disparities and optimize health care outcomes by employing the guiding principles and practical strategies of health literate care
- Demonstrates an understanding of the role of social and structural determinants of pediatric and OB/GYN disease prevention, health promotion, and health equity
Required Clinical Experiences
- Prenatal care: Assist in providing office-based prenatal care
- First trimester bleeding: Observe the evaluation of a patient with first trimester bleeding
- Normal spontaneous vaginal delivery: Assist a normal labor and spontaneous vaginal delivery
- Cesarean delivery: Assist with a cesarean delivery
- Post-partum depression screening: Perform a screen for post-partum depression
- Neonatal jaundice: Assist the evaluation of a newborn with jaundice
- Well child care-infant: Assist an infant well-child exam (age newborn to 12 months)
- Well child care-preschool: Assist a young well-child exam (age 15 to 60 months)
- Well child care-adolescent: Assist an adolescent well-child exam
- Child with chronic medical problem: Assist the evaluation of a child with a chronic medical problem (e.g., asthma, diabetes, epilepsy, cystic fibrosis, genetic syndrome)
- Pediatric cough/wheeze: Assist the evaluation of a child with cough or wheeze
- Pediatric ear pain/otitis media: Assist the evaluation of a child with ear pain or otitis media
- Pediatric fever: Assist the evaluation of a child with fever
- Pediatric gastrointestinal complaint: Assist the evaluation of a child with an active GI problem (e.g., vomiting, diarrhea, abdominal pain)
- Pediatric atypical growth or development: Observe the evaluation of a child with abnormal growth or development
- Pediatric rash: Observe the evaluation of a child with rash
- Menstrual abnormalities: Assist the evaluation of a patient with menstrual abnormalities
- Sexually transmitted infection: Assist the evaluation of a patient with a sexually transmitted disease
- Bimanual pelvic exam: Perform a bimanual pelvic exam
- Speculum exam: Perform a speculum exam
- Pap smear: Perform a pap smear
- Cervical dysplasia: Assist the evaluation of a patient with cervical dysplasia
- Cervical cultures: Perform cervical cultures
- Menopause: Assist the evaluation of patient with menopause
- Hysterectomy: Assist with a hysterectomy
- Laparoscopic abdominal/pelvic surgery: Assist with a laparoscopic abdominal/pelvic surgical case
- Breaking bad news: Observe breaking bad news to a patient
Chronic and Preventive Care
Chronic and Preventive Care is a 12-week block in Phase 2 that uniquely positions students to identify the roles of physicians, interdisciplinary providers, health care systems and communities in screening, treating and preventing common, chronic conditions. Activities are centered on health promotion, outpatient-based chronic disease management, and community health.
Students’ clinical experiences occur in primary care, behavioral health and other ambulatory and community-based settings that focus on chronic disease management. Continuity occurs in primary care clinics over the 12 weeks as well as in a longitudinal community health engagement project.
This block builds upon Phase 1 fundamental science concepts introduced in Food, Fasting and Fitness; Body in Balance; Invaders and Defense; Human Family Tree and Mind and Motion. Structured educational sessions employ varied modalities including podcasts, real-time case discussions, webcasts, independent readings and online simulation.
All students participate throughout the 12 weeks in a field experience with community health engagement.
Course Objectives
- Use effective communication skills with patients and families
- Identify and use skills that promote interprofessional and team-based care
- Participate in the care of non-English speaking patients and discuss the regulatory requirements that direct services and how language differences may lead to health disparities
- Identify skills necessary to communicate patient information with health care teams
- Describe the anatomic, pathophysiologic and epidemiologic aspects of common conditions addressed in the outpatient setting, linking basic science concepts with clinical knowledge
- Recognize limitations and benefits in the scientific process and how to identify, evaluate and apply new knowledge
- Distinguish the varying causes of common conditions addressed in the outpatient setting, including both modifiable and non-modifiable factors
- Develop a clinical strategy to evaluate and treat common medical conditions which are addressed in the outpatient setting
- Communicate effectively with patients and families to identify goals and barriers related to health and arrive at individualized treatment plans
- Demonstrate effective use of health information technology
- Make evidence-based recommendations for screening and prevention of common conditions encountered in outpatient settings
- Using self-reflection, peer feedback, and mentor feedback; continue to develop the skills and attitudes necessary for clinical practice
- Demonstrate ethical principles in obtaining informed consent
- Participate in the design, implementation, or assessment of a community health intervention
- Identify and use skills necessary to improve quality of medical care and patient safety
- Demonstrates effective communication strategies to ensure patients, families, and community members are informed of best practices related to health promotion
- Demonstrate accepting, non-judgmental behavior towards all people in all learning environments
- Demonstrate integrity, organization, and dependability in all learning environments
- Applies best practices for collaborating with communities resources to provide care for patients and populations
- Applies principles of healthcare stewardship while working to prevent and control the effects of various chronic conditions at the levels of individual patients, families, communities, and society
Required Clinical Experiences
- HEENT exam: Perform an HEENT examination of a patient
- Shoulder exam: Perform a musculoskeletal shoulder examination of a patient
- Plan of care: Communicate the plan of care with a patient
- Chronic mental illness: Assist in the evaluation, management and disposition of a patient with chronic mental illness (severe mood disorder, schizophrenia or schizoaffective disorder) by interacting with a member of the patient’s outpatient mental health system
- Imbalance assessment: Evaluate a patient with a balance complaint and develop a differential diagnosis
- Patient evaluation: Evaluate at least two patients (may be done in conjunction with one of the experiences listed above)
- Writing a prescription: Write a medication prescription accurately and safely in a clinical setting
- SBIRTs and motivational interviews: Perform at least one SBIRT and one Motivational Interview with a patient in clinic
- Dermatologic exam: Obtain a focused history and exam and formulate a prioritized differential diagnosis for a patient presenting with a dermatologic concern
- Diabetic foot exam: Obtain a focused history and perform a foot exam for a patient with insulin dependent diabetes mellitus
- Pulmonary disorders: Obtain a focused history and exam and formulate a prioritized differential diagnosis for a patient presenting with a pulmonary concern
- MSK/rheumatological history: Obtain a focused MSK/rheumatological history in a clinical setting
- Substance use: Incorporate screening for substance use disorders as a routine part of clinical practice using evidence-based screening tools
- Patient preferences: Incorporate patient preferences when discussing prevention guidelines
- Religion and spirituality: Address aspects of a patient’s religion or spirituality that impact his or her health and health care in a clinical setting
- Metabolic disorder counseling: Counsel patients on behavioral strategies and recommend appropriate treatment to minimize morbidity due to different types of metabolic disorders
- Mental health counseling: Counsel patients on behavioral strategies and recommend appropriate treatment to minimize morbidity due to different types of mental health disorders
- Interpreter use: Assess a patient for the need of an interpreter
- HealthLink: Use HealthLink (or other clinical decision support) during patient care and demonstrate the integration of information technology into the process of clinical care, especially clinical decision-making
- Patient instructions: Demonstrate the ability to generate thorough and understandable patient instructions in the after-visit summary
- X-rays: Demonstrate a systematic approach for interpreting skeletal X-rays
- Diagnostic tests: Order common diagnostic tests for core clinical conditions in clinical settings
Resident Video
Acute Care
Acute Care is a 12-week block in Phase 2 that is centered on assessing patients with urgent medical conditions, providing acute inpatient care and transitioning patients to other care settings or home under the care of other professionals.
Activities emphasize providing acute care in outpatient emergent and inpatient ward settings, developing acute management plans and subsequent transition of care plans. Clinical experiences are in acute care settings.
The block builds upon the fundamental science concepts introduced during Phase 1, including acid base balance, hormonal regulation, cardiac physiology and infection. Structured educational sessions proceed through the 12-week block following an organ system-based approach and employ varied modalities including podcasts, real-time case discussions, webcasts, independent readings and online nationally supported modules.
All students complete an integrated patient-centered experience by participating in the care of a patient from an urgent admission through inpatient treatment and discharge.
Course Objectives
- Explain the anatomy, physiology, biochemistry and pathophysiology as it relates to imaging and patient conditions
- Describe the impact of social and economic factors on the clinical management of individual patients
- Provide care to acutely ill adult patients by using clinical and physical exam findings and test results to develop and prioritize a differential diagnosis and treatment plan
- Use interpersonal communication skills to provide effective medical care
- Use an electronic health record
- Use evidence-based practices in patient care
- Demonstrates effective communication strategies with a variety of audiences, including patients, families and colleagues, to convey evidence-based health care guideline or policy recommendations
- Engages in scientific inquiry to synthesize and apply emerging evidence to provide care for patients with acute illness
- Use self-assessment and feedback to establish goals for future practice
- Demonstrate integrity, organization, and dependability in all learning environments
- Contribute to the learning process as a member of the patient care team
- Demonstrate professionalism during every clinical encounter
- Identify and use skills necessary to improve quality of medical care and patient safety
- Identify policy interventions that impact health outcomes
- Applies principles of resource stewardship and cost considerations when delivering patient care
- Demonstrate effective communication using oral, written and electronic formats to establish and maintain collaborative relationships with patients, families and communities
- Demonstrates effective communication using oral, written and electronic formats to establish and maintain collaborative relationships with members of the interprofessional team
- Consider how bias and stigma affect health outcomes for diverse populations
- Effectively communicates information in small group settings to colleagues and peers using oral, written and electronic formats
Required Clinical Experiences
Core clinical conditions: Students will participate in the care of patients with core clinical conditions:
- Myocardial infarction
- Atrial fibrillation
- Sepsis
- Pneumonia
- Heart failure
- Respiratory distress
- Suspected venous thromboembolic disorder
- GI bleed
- Liver disease
- Glucose disturbance
- Stroke/TIA
- Altered mental status
- Blood pressure disturbance
- Syncope
- Suicidal ideation
- Behavioral disturbance
- Acute Kidney Injury
- Electrolyte Imbalance
- Medication reaction
Resident Video
Surgical and Procedural Care
Surgical and Procedural Care is a 12-week block in Phase 2 focused on the care of adults and children undergoing an operation or procedure, including the perioperative preparation, operative care and post-operative cares for core clinical conditions in the specialties of anesthesia, neurosurgery, ophthalmology, general surgery, otolaryngology, urology, cardiothoracic surgery, peripheral vascular surgery, orthopedics, plastic and reconstructive surgery and gynecology, as well as interventional radiology, procedural cardiology and gastroenterology.
The block builds upon the basic science concepts introduced in Phase 1, including cerebral spinal fluid production and flow, fluids and electrolytes, consciousness, inflammation and wound healing and cancer biology.
Patient care experiences take place in the clinics, emergency department, inpatient wards, inpatient and outpatient operating rooms and procedure suites. Structured educational sessions proceed through the 12-week block following an anatomic approach using case discussions, podcasts, curated independent reading, online nationally supported modules and simulation skills.
All students complete a longitudinal patient care experience by participating in the pre-operative preparation, anesthesia care, operative care and post-operative care of one inpatient.
Course Objectives
- Communicate effectively with assigned patients and their families
- Identify and uses skills that promote interprofessional and team-based care
- Identify the role of personal biases and morals in influencing patient care
- Model accurate, clear, and concise oral and written presentations
- Relate anatomy to the pathophysiology of core clinical conditions and apply knowledge of anatomic relationships, therapeutics, and prevention to the care of patients
- Explore the role of social determinants on the health outcomes of patients
- Demonstrate a comprehensive approach to the care of adult and pediatric patients
- Discuss important findings, management, treatment and prevention options with patients and families
- Demonstrate effective use of health information technology
- Participate in providing care to adult and pediatric patients who require common procedures as part of their medical care
- Access, analyze and evaluate scientific and medical literature to address learning needs and apply current evidence to patient care
- Seek out feedback from teammates and supervisors and use it to engage in ongoing self-assessment of knowledge, skills and attitudes
- Demonstrates honesty and dependability in team-based work, engages in activities to improve ability to prioritize and manage time effectively
- Demonstrate legal and ethical principles with patients, specifically as it pertains to the informed consent process
- Identify and use skills necessary to improve quality of medical care and patient safety
- Identify appropriate ways to provide patient care in a resource limited setting
- Demonstrates effective communication strategies with a variety of audiences, including patients and families, to convey evidence-based recommendations, including discussions around surgical consent and pre- and post-operative health care recommendations
- Engages in scientific inquiry to synthesize and apply emerging evidence to provide care for surgical patients
- Demonstrate accepting, non-judgmental behavior towards all people in all learning environments
Required Clinical Experiences
- Abdominal pain: Participate in the care of a patient with abdominal pain
- Colorectal or anal disease: Participate in the care of a patient with colorectal or anal disease
- Hepatobiliary disease: Participate in the care of a patient with hepatobiliary disease
- Consent: Observe at least one instance of informed consent, paying particular attention to communication skills, potential for bias, and physician/patient power imbalance during the interaction
- Gown and glove: Gown and glove in sterile environment
- Suture skills: Suture and tie knots
- Trauma: Participate in the care of a trauma patient
- Multi-D conference: Observe or participate in multidisciplinary conference (e.g., tumor board, multi-D cancer management conferences, vascular anomaly working group, multi-D discharge planning)
- IV catheter: Place an intravenous catheter (must be performed no less than three times)
- Airway management: Manage a patient airway, including mask ventilation and either laryngeal mask airway (LMA) or endotracheal tube placement (must be performed no less than three times)
- Multiple exams: All students are expected to participate in the care of at least four patients with one or more conditions:
- Ear pain
- Throat pain
- Neck mass
- Joint disease
- Back or neck pain
- Spinal disease
- Peripheral arterial disease
- Venous disease
- Cardiac disease
- Lung disease
- Skin and/or soft tissue disease
- Breast disease
- Benign genitourinary disease or injury
- Malignant genitourinary disease or injury
- Eye disease
- Intracranial mass